Treatment of Bites and stings in A&E
- Robert Bradley

- Aug 11, 2024
- 3 min read

Lets work together to avoid antibiotic resistance
We often have people turn up to our urgent care center with insect bites. These can become very swollen red and inflamed soon after being bitten. It is commonly mistaken for an infection.
NICE Guidelines state that a rapid onset skin reaction including erythema, heat and swelling from an insect bite or sting is more likely to be an auto-immune response rather than an infection. Most stings or bites will not require antibiotics.
This is caused by the syliva/poison that has been injected into your body causing your immune system to respond. Often, your body’s immediate response will include redness, heat and swelling at the site. Minor delayed reactions can include itching and soreness.
In the history take try and get as much information as possible
1. Do they have a history of bad reactions to insect bites?
2. Where have they been in the last 24 hours? (indoor/outdoor/garden/woods/fields/ponds/swimming outdoors)
3. Any pets?
4. Any one else been bitten?
5. Are they immunocompromised?
Consider an Auto-immune response if:
Presented <72 hours of bite/sting
Redness, heat and swelling
Itching
Vomiting
Diarrhoea
Fever lasting <24 hours after bite (usually under thirty nine degrees celcius)
Pain around site of bite
Signs of Anaphylaxis
Bruising
Malaise
Large hives
Consider Antibiotics if:
Presented after >72 hours of bite/sting
Persistent Redness, Heat and swelling >72 hours
Persistent fever >24 hours
Patient is immunocompromised
Yellow/green exudate (puss)
Persistent pain >72 hours or severe pain out of proportion to wound
Redness is spreading
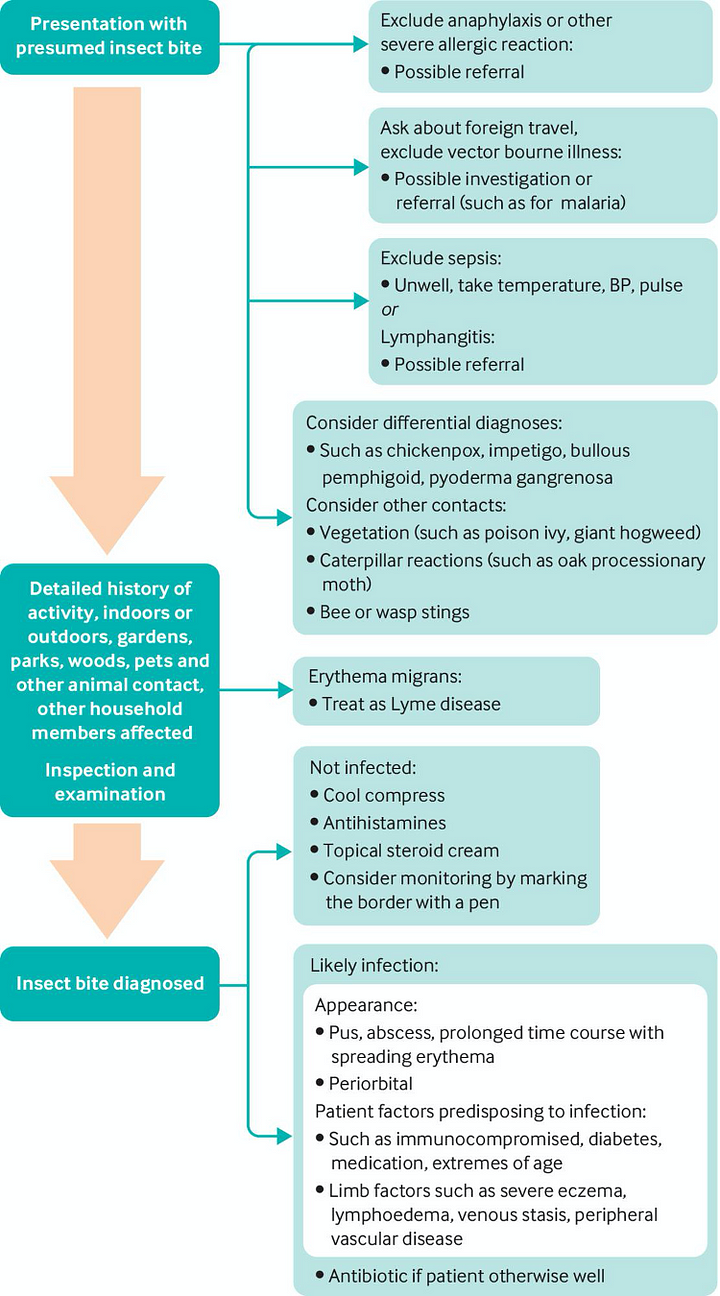
A helpful tool found in the BMJ:
BMJ 2020; 370 doi: https://doi.org/10.1136/bmj.m2856 (Published 07 August 2020)Cite this as: BMJ 2020;370:m2856
Another useful tool from NICE:

Treatments for non-infected insect bites/stings:
Remove the sting, tick or hairs if still in the skin.
Wash the affected area with soap and water.
Apply a cold compress (such as a flannel or cloth cooled with cold water) or an ice pack to any swelling for at least 10 minutes.
Raise or elevate the affected area if possible, as this can help reduce swelling.
Avoid scratching the area or bursting any blisters, to reduce the risk of infection — if your child has been bitten or stung, it may help to keep their fingernails short and clean.
Avoid traditional home remedies, such as vinegar and bicarbonate of soda, as they’re unlikely to help. Important considerations
Topical steroids and antihistamines may help and your pharmacist can help with this
Draw around the redness to check if it is spreading
IMPORTANT CONSIDERATIONS
Necrotising Fassciitis
If patient appears very clinically unwell, appears septic, rapidly progressive erythema, blistering, pain that is out of proportion to wound and fever consider Necrotizing Fasciitis and seek senior advice urgently
There are tools available to assess the risk of this including:
Tetanus status
Another important issue to consider after an insect bite is Tetanus status. Insect bites or any dirty breaks in the skin can infect you. You should have a booster every 10 years unless we can prove that you have immunity still. We have a device in our urgent care centre that can check if you still have immunity which is very useful and prevents unneccesary vaccinations.
A course of 5 Tetanus vaccinations usually provides life long lasting cover but if it has been over 10 years it is still worth getting checked out for immunity.
Symptoms of Tetanus include:
Stiffness in the jaw muscles, painful muscle spasms that can affect swallowing and breathing, fever, sweating and a rapid heartbeat.
N.I.C.E. recommends for clinicians to advise people that present with an insect bite or sting that:
A community pharmacist can advise about self-care treatments
2. Skin redness and itching are common and may last for up to 10 days
3. It is unlikely that the skin will become infected
4. Avoiding scratching may reduce inflammation and the risk of infection
5. They should seek medical help if symptoms worsen rapidly or significantly at any time, or they become systemically unwell.
I hope you found this helpful. Please feedback any issues you have had so we can share learning experiences and make us all better clinicians.




Comments